It is frustrating and heartbreaking to see someone you care about slowly change and not be able to do anything about it. Researchers all over the world are working to find answers to help stop or slow dementia. What is hard to accept is that it takes time. It will take many discoveries, and as they build upon one another over time, there will be successful treatments.
The focus for current research on Alzheimer’s and other dementias is:
• the study of the brain and interaction of brain cells and their breakdown
• methods for earlier detection and monitoring of disease progression
• drug development and other non-drug interventions along with human trials
• the study of potential health factors that may impact the risk for dementia
• examining lifestyle factors that could impact the risk for dementia
• work to bridge the gap between research discoveries and therapeutic development.
Every day new discoveries are made. The following are the most recent research advancements as of February 2024.
Detection
Biomarker tests which help measure changes in the brain associated with the disease are widely used by researchers in the lab, such as the PET scan or blood tests. And a possible new way to detect Alzheimer’s Disease has been discovered by an international research team funded by Bright Focus Alzheimer’s Disease Research program. They recently developed an AI model to study and compare details in photos of the retina of the eye. It is an expectation that, one day, these tests will be used by doctors in a clinical setting.
Drugs to Stop the Progress of Dementia
The primary hallmarks of Alzheimer’s disease are: Amyloid plaques, Tau tangles, and Neurogeneration. A new category of drugs for the treatment of Alzheimer’s, known as monoclonal antibodies, have been developed which target the clumps of beta-amyloid in the brain and help remove these protein-based plaques which are known to kill healthy neurons in the brain. Some have had mixed test results, but one monoclonal drug has been shown to slow cognitive decline by 25%. Lequembi was granted full approval by the U.S. Food and Drug Administration to treat individuals with earlier stages of mild cognitive impairment or mild dementia. There can be some flu like reactions due to the infusion mode of administering the drug, and swelling or small bleeds in the brain have occurred in rare instances. Whether to to take the drug depends on your health background. The challenge now, for researchers, is to find a way to untangle the Tau tangles.
Treatment Cross-over
Researchers are also looking into treatments and vaccines already in use for other diseases to see if they can be effective on dementia. There is evidence that brain health is closely related to heart and blood vessel health. The risk of developing dementia is seen to increase as a result of conditions that cause damage to the heart and arteries such as heart disease, high blood pressure and high cholesterol. Researchers are looking into whether medicines to treat these conditions may decrease the risk or slow the decline of memory associated with dementia. Insulin therapy and hormone replacement have not found success, but a study by a research team at Duke University Social Science Research Institute shows promise. They investigated associations between pneumococcal vaccination and the risk of Alzheimer’s disease, and found that a vaccination between the ages of 65-75 reduced risk for developing the disease by 25-30%, adjusting for other factors. Lead researcher Svetlana Ukraintseva, Ph.D. said, “These data suggest that pneumococcal vaccine may be a promising candidate for personalized Alzheimer’s prevention.”
Exposome
An area that has gained much interest in the research community is an environmental health approach to Alzheimer’s and dementias. Over the course of a person’s life, they are exposed to environmental factors such as the food and water they ingest, the air they breathe as well as social and psychological environments they experience. The totality of these environmental exposures that have a direct effect on human health is called the exposome. Environmental toxicants like air pollution, pesticides and metal toxins have been linked to several neurogenitive disorders including dementias and have been seen to disproportionately affect poorer communities. With the advancement of computing it is now possible to measure the aspects of the exposome and their relationship to human health. How they affect the risk for dementia is still being studied.
Genomics
Genomics has made a huge advancement, biomedical research in recent years. Studies of the genome has led to identifying the genetic basis of many complex diseases. Genome-wide Association Studies (GWAS) conducted as part of the Alzheimer’s Disease Sequencing Project (ADSP) were successful in identifying 70 regions of the genome associated with Alzheimer’s along with genetic variations that may play a role in the role of AD. As yet, how these genetic regions affect the function of molecules or cells in the body or confer risk for dementia is still unknown.
Individual Cells
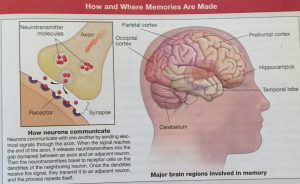
The study of AD and dementia is set to expand to the analysis on the scale of individual cells. The techniques, advanced by Brain Research Through Advancing Innovative Neurotechnologies (BRAIN) “can facilitate comparisons across cells” and “can help shed new light on disease dynamics.”
Final Thoughts
While we would like to see a speedy break-through discovery of a treatment that would eliminate the causes and continued impairment of the brain from Alzheimer’s and other dementias, know that this goal is also shared by scientists and researchers. What is key to the finding a treatment is cooperation and sharing between those who are involved in the research. An example of this is the consortium CPAD, formed under the direction of the National Institute on Aging to share data from clinical trials. Consortium partners include pharmaceutical companies, non-profit foundations and government advisors.
The scientific and medical community now realizes there will probably be no one drug or therapy that will be successful for those who suffer with AD or dementia. In the near future, researchers expect a range of treatments and approaches tailored to each individual, similar to the way we treat cancer today.
Information obtained from:
National Institute on Aging www.nia.nih.gov
Bright Focus Foundation www.brightfocus.org
Alzheimer’s Association alz.org